
Dr Vijay Anand Ismavel and Dr Ann
Doctors out there: Why small hospitals matter
Civil Society News, New Delhi
In 1992 a young couple, both doctors, travelled from Madurai in Tamil Nadu to a remote corner of Assam to check out the Makunda Christian Leprosy and General Hospital. They had been told that the hospital needed to be revived, having become defunct 10 years earlier after the missionaries running it were asked to leave India.
Vijay Anand Ismavel had a master’s in surgery and Ann, his wife, was an MBBS physician. With qualifications like theirs, getting jobs or setting up a practice was easy. There was really no great need to leave Madurai. Both of them, however, had other expectations from their profession. They wanted to take their medical skills to the people who needed them the most — the farther away and the larger the number the better.
When they turned up at the Makunda Hospital they found it was just the kind of challenge they were looking for. It was in a decrepit state, located on grounds over hundreds of acres and it had a vast catchment of under-served poor rural people.
The Emmanuel Hospital Association (EHA) was ready to support the revival of the Makunda Hospital provided it could find someone who would make a long-term commitment to transforming it into a modern facility. It meant living and working there for as long as it would take.
No two worlds could have been more apart than Madurai and Bazaricherra, a neglected corner of Karimganj district, where the Makunda Hospital was located. But Vijay and Ann, then in their 20s, were excited about making the transition. They told the EHA that they were ready to commit the next 30 years of their lives to the remaking of the Makunda Hospital.
Now in the 28th year of that commitment, the Makunda Hospital offers a range of services with a degree of quality, rigour and affordability that many big-city hospitals might find difficult to match. Its records for 2018-19 show it received 100,000 outpatients and 17,000 others who were given admission. It conducted 6,000 deliveries and 3,000 major surgeries.
As India staggers under the challenges of dealing with a brutal coronavirus pandemic, the shortcomings in its healthcare infrastructure now show up more starkly than ever. The millions of migrant workers who filled TV screens recently, as they tried to flee cities, really have nowhere to go for treatment, especially once they are back in their villages.
 Perhaps this is a particularly appropriate time to learn from the experience of successful small hospitals like the Makunda Hospital in the not-for-profit sector. Many innovative models for public healthcare can be found among such spirited institutions. They not only fill gaps in the healthcare system, saving lives and improving health indicators, they also show how standards can be kept high without unreasonably raising costs or extracting profits. Through the zealous efforts of people who work in them, these hospitals also take the medical profession back to its original moorings of dedication and selflessness.
Perhaps this is a particularly appropriate time to learn from the experience of successful small hospitals like the Makunda Hospital in the not-for-profit sector. Many innovative models for public healthcare can be found among such spirited institutions. They not only fill gaps in the healthcare system, saving lives and improving health indicators, they also show how standards can be kept high without unreasonably raising costs or extracting profits. Through the zealous efforts of people who work in them, these hospitals also take the medical profession back to its original moorings of dedication and selflessness.
The EHA has in its fold 21 hospitals like the Makunda Hospital in remote parts of India. Much beyond the EHA, Christian mission hospitals, both Protestant and Catholic, are said to account for 60,000 beds, once again in places where they are much needed.
Similarly, there are the Ramakrishna Mission hospitals that work within communities and provide affordable care. There are also some 400 well-qualified rural surgeons who have chosen to open hospices in remote parts of the country, performing general surgeries at low cost. A great example of the Rural Surgeons’ Movement is the Rural Medicare Centre at Saidulajab in the periphery of south Delhi. Dr JK Banerjee and his wife began it in a tin shed and today, having blossomed into a hospital with modest charges, it receives throngs of patients. Dr Banerjee is no more, but several competent physicians and surgeons try to keep his dream alive. Such medical skills might otherwise have been unreachable for the poor patients with small incomes who go there. (Read Dr Banerjee's obituary here)
There is also Doctors for You (DFY), a team of physicians, which swings into action when there are emergencies. In addition to their rapid-response services, these doctors have also set up a 30-bed hospital, to be expanded to 200 beds, in Bihar. And in Bilaspur you would find the Jana Swasthya Sahyog.
The list of such efforts is a long one. Each effort is impactful in its own way. In Civil Society magazine, as journalists, we have done stories on them over the years, getting to know the doctors and understand what their hospitals do. But nationally, in terms of policy and government outreach, not enough is done to use them to enliven and strengthen the national healthcare system.
PARTNERSHIPS
“Creative partnerships are the way forward and the government must learn to draw on talent and experience in the non-profit sector as well as the best of the private sector to create healthcare infrastructure in smaller cities and villages apart from strengthening hospitals in the big urban centres,” says Dr Ravikant, 40, founder of DFY. (He prefers to be known only by his first name.)
Dr Ravikant, who is currently camping in Muzaffarpur in Bihar to set up a cancer hospital with government support, calls for a reset in values and priorities among medical professionals and in the healthcare system as a whole. He emphasizes the role of public health specialists. There should be incentives, he says, for taking degrees in public health and it should be a mandatory qualification for doctors in administrative roles. (See our story on Dr Ravikant from September 2018)
DFY has engaged with government hospitals in several states and tried to improve their processes and standards. Motivating government doctors has been part of this effort. But institutionalized steps are needed for such engagements to have a lasting impact. DFY teams are compelled to gingerly nudge government doctors and other staff in the direction of improvements. It doesn’t take long for them to slump back into their old ways. The coronavirus pandemic has underlined the need for governments to act decisively on improving systems and raising standards in their facilities. (Also read about DFY's work in TB hotspots)
 “There should be lateral entry into the government healthcare system,” says Dr Ravikant. “We should also consider having a cadre called the Indian Public Healthcare Service along the lines of the Indian Administrative Service where talented young doctors can join and strengthen the government system.”
“There should be lateral entry into the government healthcare system,” says Dr Ravikant. “We should also consider having a cadre called the Indian Public Healthcare Service along the lines of the Indian Administrative Service where talented young doctors can join and strengthen the government system.”
“We need to decentralize healthcare and go to the smaller cities and towns. Kerala has done well during the current pandemic because it has a healthcare system that goes all the way down to the grassroots. You need people to survey, test, quarantine and so on,” he explains.
But Kerala is an outlier. Generally, the government systems in most states are not as responsive. From primary health centres to district hospitals and specialty facilities, linkages are either weak or don’t exist. General hospitals run by the government are, with some exceptions, in a shambles. Private hospitals are too commercial.
THREE PHASES
The non-profit sector, on the other hand, shows what can be achieved at ground level and in remote locations. To return to the Makunda Hospital example, when Vijay and Ann started out in 1993, a year after their first visit, they drew up a strategic plan, which consisted of three phases of 10 years each.
They have ensured that the Makunda Hospital is sustainable, earning what it spends except for one or two percent of its revenue that comes from donors. In fact, the hospital spends `3 crore of its own earnings by way of charity, which essentially means treating poor patients free.
The hospital has motivated staff and a succession plan is under way with replacements for the Ismavels ( Vijay is 56 and Anne 53) already in position. In addition to the services the hospital provides at its original location, it has a branch in Tripura and outreach in its own radius, thereby reaching people where they live and creating healthcare awareness.
 Vijay and Ann have also set up a school attended by 1,200 students from the same catchment that their poor patients come from. Health and education have gone together and brought awareness and empowerment to people who now not only have a hospital they can rely on but also know what better health is about.
Vijay and Ann have also set up a school attended by 1,200 students from the same catchment that their poor patients come from. Health and education have gone together and brought awareness and empowerment to people who now not only have a hospital they can rely on but also know what better health is about.
While the government struggles to get good doctors to rural areas and small cities, the Makunda Hospital succeeds in attracting talent ready to work for modest salaries.
“There is a disproportionate number of healthcare workers in urban and richer parts of the country. Although work in the more remote parts is not so glamorous or rewarding from the material point of view, it is certainly more challenging and fulfilling. This needs to be told to young medical professionals, so that some of them would consider working in such places at least as part of their career and do so joyfully and not as a burden,” says Dr Vijay Ismavel.
He emphasizes partnership with the government as being essential for any large-scale impact. “Most hospitals are capable of local impact on their own but partnership with the government allows regional impact. It is important to engage, for thought-sharing and understanding each other’s constraints and closing gaps based on each other’s strengths,” he says.
But problems exist with policies and laws, which do not take into account the needs of people and hospitals in remote rural areas.
“The challenges and constraints in rural areas are different. Healthcare indices can be quickly improved with the minimum of investment. Hospitals in such places should get incentives as well as relaxations and exemptions from stringent requirements — not to lower quality but to be realistic,” explains Dr Ismavel.
POLICY HURDLES
For all the great work they do, small and remote hospitals are not adequately consulted during discussions on framing national healthcare policies. Large hospitals, whether owned by the government or private corporations, on the other hand, have little problem being heard and defining policy. They hog regulatory space. This is unfortunate because they have little interest in rural areas.
“Government facilities in many grassroots areas are not good and may vary a lot from state to state and corporate interest is poor in such areas as there’s not much money to be made. It is the non-profit hospitals that are important for closing the gap between those who can and those who can’t access quality affordable healthcare,” says Dr Ismavel.
The rules relating to blood banking are an example of the hurdles small hospitals face. Hospitals need ready access to blood during emergencies, but only a registered blood bank can draw blood from a donor.
To get a licence for setting up a blood bank a hospital has to have on its staff a pathologist or an MBBS medical officer with at least one year of experience in a blood bank. It is difficult to get either in a remote rural location. The Makunda Hospital has had to settle for being a ‘blood storage centre’ but if it runs out of blood and needs it during an emergency, the hospital has to get it from a blood bank 50 km away.
Says Dr Ismavel: “Hospitals requiring large amounts of blood in remote rural areas should be allowed to have a blood bank with trained doctors and good standards but with relaxation of stringent rules — maybe a doctor who has worked for a month in a reputed blood bank and with the hospital having excellent protocols and practices in place — which can be inspected and approved.”
 Another example of a policy hurdle is that under the Assam Clinical Establishments Act, to conduct deliveries the Makunda Hospital was required to have a full-time obstetrician, pediatrician, physician and anesthesiologist. Since it didn’t have this level of staffing for each delivery, the hospital received a closure notice.
Another example of a policy hurdle is that under the Assam Clinical Establishments Act, to conduct deliveries the Makunda Hospital was required to have a full-time obstetrician, pediatrician, physician and anesthesiologist. Since it didn’t have this level of staffing for each delivery, the hospital received a closure notice.
“We requested time and now have all these consultants. However, if the hospital had been forcibly closed at that time, thousands of patients from a large and remote rural area with limited options would have been severely affected,” recalls Dr Ismavel.
SURPRISE DECISIONS
Collaborations with governments can be fraught with uncertainties. In Hyderabad, Dr Evita Fernandez, a gynaecologist who runs the Fernandez Hospital, took up the training of 30 nurses from five states under the National Midwifery Educators’ Programme. An understanding was signed with the University of Lancashire to bring in five international midwifery educators.
The programme was successfully underway when the Telangana government withdrew its support because the National Health Mission director in the state changed and the new incumbent didn’t think the programme was necessary. (Read our story on Dr Evita Fernandez from September 2012)
Similarly abandoned was a programme for setting up palliative care centres for cancer patients in the districts of Telangana. It was supported with funds from the Union government and six centres were set up through an interesting partnership between the state government and voluntary organizations in India and abroad. All six centres have been closed. (Read our story on Telangana's palliative care centres here)
“It is not easy to work with the government when a single officer can take a decision which is impossible to reverse. It is a lot of effort wasted. We shifted training of nurses to the Fernandez Hospital, but the idea was to conduct the training in a large government hospital. We have also been left paying a rent of Rs. 3 lakh a month for a building where the nurses were accommodated,” says Dr Fernandez.
 Dr Fernandez says non-profit and mission hospitals have an important role to play in primary and secondary care. She feels the government should institutionalize them and support them with subsidies for electricity, water and equipment. They should have access to concessional finance.
Dr Fernandez says non-profit and mission hospitals have an important role to play in primary and secondary care. She feels the government should institutionalize them and support them with subsidies for electricity, water and equipment. They should have access to concessional finance.
Dr Fernandez has added two hospitals to the original Fernandez Hospital, which her parents set up. All three are in the private sector but are run with a social heart.
“Our doctors don’t live in mansions but they get comfortable salaries. They aren’t given any incentives,” she says.
Rich patients subsidize the poorer ones and no one is turned away unless there just isn’t a bed or the case is beyond the hospital’s competence.
DOCTORS’ SALARIES
The business model of a hospital defines the medical standards that a patient can hope for. When profit is the motive, medical standards tend to take a hit. In insidious ways a work culture develops in which making money becomes all-important. It is a slippery slope.
Government hospitals aren’t into chasing profits, but they tend to get mired in corruption, lack motivated doctors and generally deliver poor care though there are exceptions and a state like Kerala shows what the government sector can achieve.
Non-profit hospitals that discipline themselves and become sustainable from their own revenues seem to strike the right balance. They are neat and clean and stick to the essentials. No fancy rooms and marble floors.
What doctors earn is key to achieving this balance. At Makunda and other EHA hospitals, an MBBS physician gets around Rs. 32,000 and an MD Rs. 46,000 when starting out with annual increments to follow.
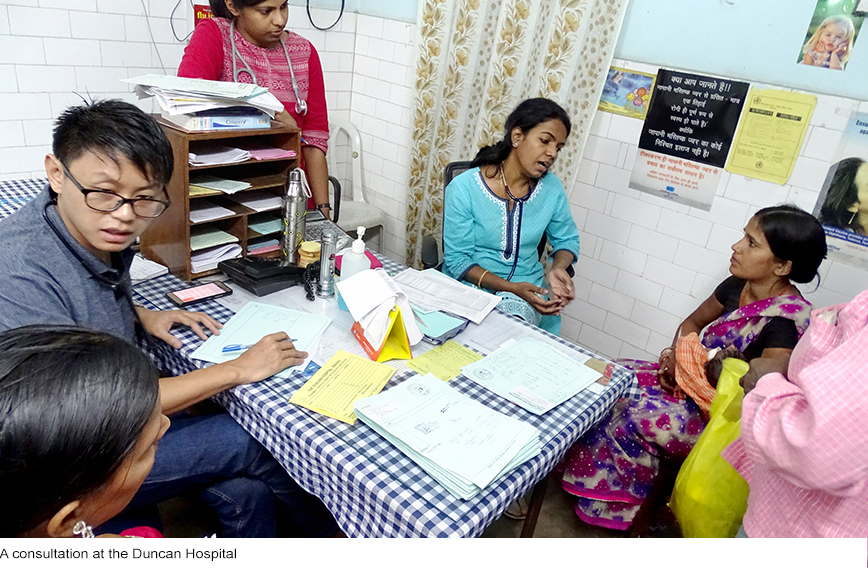
Even after 28 years at the Makunda Hospital, Dr Ismavel gets Rs.1.25 lakh and Ann gets around Rs. 95,000. At the Duncan Hospital, at Raxaul in Bihar, also part of the EHA, Dr Prabhu Joseph, 42, a spinal surgeon who also serves as the superintendent, gets Rs. 71,000 and his wife, Blessy, 41, a paediatrician gets Rs. 58,000. Such salaries are enough to live comfortably and even have some savings in rural locations though they are nowhere near what commercial hospitals pay in big cities.
Both the hospitals are sustainable and the jobs they offer are stable. The Duncan Hospital’s annual income is Rs. 21 crore out of which it does Rs. 1 crore of charity. The Makunda Hospital earns around Rs. 20 crore annually and does Rs. 3 crore of charity.
Doctors are able to dedicate themselves to medicine. The experience they get is both satisfying and great for their careers. Dr Joseph recalls that when he came to the Duncan Hospital after getting his MBBS degree in Belgaum, he operated on a woman patient with a perforated abdomen. He wouldn’t have got that opportunity elsewhere. Additionally, he found role models in doctors like Santosh Mathew and his wife, Saira, who had in their younger days similarly chosen to serve in rural areas.
 Both Dr Joseph and Dr Ismavel, as well as their wives, have gone on to acquire postgraduate degrees at the Christian Medical College in Vellore after working at these rural hospitals. Their experience has made these degrees more meaningful.
Both Dr Joseph and Dr Ismavel, as well as their wives, have gone on to acquire postgraduate degrees at the Christian Medical College in Vellore after working at these rural hospitals. Their experience has made these degrees more meaningful.
“Normally young doctors are goaded by their families to immediately go in for postgraduate degrees. After that they begin chasing a living. It is much better to first work a few years, particularly in a rural area,” explains Dr Ismavel.
“After a few years here, I specialized in pediatric surgery at the Christian Medical College in Vellore. When I returned, I was the only pediatric surgeon in the southern half of the northeast. In Chennai at that time if there were 60 pediatric surgeons and I would have been the 61st,” he says, emphasizing that the real opportunities for doctors as well as the need for their skills exist outside the big cities.
During the coronavirus pandemic small hospitals like Duncan and Makunda are standing by to handle a possible overflow of cases. But will the pandemic lead to an better role for them in the country’s healthcare system? More important, will young doctors be incentivized to find in these hospitals the inspiration to view their profession differently?
Comments
-

Dr. Ian D'Souza - Nov. 22, 2023, 12:58 p.m.
I was recently on a birding trip to Dosdewa when I fell and sustained a serious fracture of my left ankle. I was taken to Makunda Hospital and was extremely impressed not only with the quality of care but also the empathy shown by the doctors and staff. Keep it up guys!
-

Dr Jacob John - Feb. 22, 2022, 8:29 p.m.
Bringing the large network of not for profit hospitals under PMJAY can bring in a sea change.PMJAY is a successful and sustainable financial model for these hospitals.NITIAYOG has brought out a document on this. Dr Jacob John MS M.Ch Director Medical Services Ashtamudi Hospital and Trauma Care Centre ,Kollam Kerala
-

Hussain Ahmed - Sept. 27, 2021, 8:41 a.m.
Really very helpful hospital
-

JAWAHAR SUBBIAH - Sept. 11, 2020, 10:40 p.m.
‘Assuredly, I say to you, inasmuch as you did it to one of the least of these My brethren, you did it to Me.’ Mat 25:40. I am overwhelmed by the dedication and pursuit of these wonderful doctors. May God bless them. I had the opportunity to live in Sambalpur Orissa in late 70's and in Guwahati, Assam, in the years 2000-02. I know the difficulties in getting things done in these places. The article is a great source of motivation for the young doctors.
-

F.A.Choudhury - Aug. 18, 2020, 1:10 p.m.
Staff behavior is not satisfactory
-

Ranjit Rtanaike - May 17, 2020, 12:27 p.m.
Thank you for this wonderful article, focussing on unsung heros and heroines, who have dedicated their lives to God's work. I was blessed and privileged to meet Ann and Vijay Anand at their hospital. They are remarkable and humble, seeking nothing for themselves. Their joy is the joy of others who have received their help and that of the wonderful supporting staff. I hope the Government of India honours them, primarily so that others may know of them and be inspired by them, their faithfulness and the knowledge and proof that God is love.
-

Joseph George Anjilvelil - April 28, 2020, 3:59 p.m.
Service as this in rural areas is born of requisite empathy from the service provider. If doctors can balance this with a mindful scan of their environments, they may begin to assert their needs in novel ways too. Credit to such journalism that depicts such a need.
-

Evita Fernandez - April 28, 2020, 1:50 p.m.
I salute the doctors, nurses and support staff who have invested the best years of their professional lives to serve the underprivileged. Each one of them is an unsung hero/heroine. Thank you for this article that helps raise awareness about their work and commitment. AFter COVID-19, I hope the government will set up a partnership where these rural-based mission hospitals can be regarded as vital members of the national health service. These hospitals need to be recognised and supported.
-

Lita De Jesus - April 27, 2020, 6 p.m.
Praying for you doctors . You are the extension of God’s healing hands . JESUS loves you .
-

Dr parmod singh - April 25, 2020, 7:56 p.m.
Excellent sir
-

Subodh Dhanawade - April 25, 2020, 3:31 p.m.
A very good testimony to young doctors. To serve the needy, to serve unconditionally, is an ideal example essential in these times.
-

Jane Samraj - April 25, 2020, 2 p.m.
I knew Dr Ann when she was doing her MBBS in Madurai.She had a missionary zeal even in her student days and continue to serve the poor and the neglected along with her family. May the Lord continue to bless and keep them to serve
-

Giovanni Gnanadurai - April 25, 2020, 11:26 a.m.
I already know Vijay and Anne personally, though I do not know the younger couple in Raxaul. I have other friends and relatives working in Raxaul. I am writing to appreciate the good work Civil Society is doing. Great work over several years, bringing to the notice of the Civil Society a lot of good work going on all over the country. Keep going, and like Vijay Anand Ismavel find people to carry on the good work you are doing. And think big. Why not a TV channel on the lines of the magazene. Start with regular programmes once in a week or even a month, and then take it forward
-

RAJESWARA RAO - April 24, 2020, 6:09 p.m.
Doctors like Dr. Ismavel, and Dr. Joseph should be asked to teach their experiences in medical Colleges at once in a month. Government should think of such plans to bring great doctors like these in to medical colleges to sensitise young medical graduates of the vast opportunities in rural India.
-

Bikash Raj Adhikari - April 24, 2020, 6:06 p.m.
Good Job, Dr Vijay, Dr Prabhu and everyone at Duncan and Makunda hospital!
-

Priyanka Kadam - April 24, 2020, 5:58 p.m.
A very well researched article. I know Dr Vijay Ismavel and admire the outstanding work that he and his wife, Dr Ann have done in their lifetime. Was great knowing about the works of other doctors in our country also. Thanks for writing this. Priyanka Kadam, President and Founder, Snakebite Healing and Education Society. Website: www.she-india.org
-

Edward Vasanth Kumar - April 24, 2020, 4:22 p.m.
Dear Vijay and Ann Read the article. The service rendered by both of you are exemplary in the eyes of our Lord and Savior Jesus Christ. May God bless you both and give you health to carry on the good work.. Regards Edward 9487900964



